Medical Center » Services » Inpatient Rehabilitation
The Inpatient Acute Rehabilitation Unit at Hutchinson Regional Medical Center is dedicated to patients who have experienced a significant decline in function and who need and tolerate an intense multidisciplinary approach for their recovery. Depending on your diagnosis, the multidisciplinary team may include:
We work hard to help all patients reach the highest possible level of recovery, assisting the patient to regain and maintain independence. We also teach patients alternative techniques, when deficits remain, to perform daily tasks necessary to live successfully and safely in the community.
RehabTracker is a person-centered mobile app that allows us to better engage with our patients and their families. Patients can view their personalized goals, see and track their progress in real time, share that progress with invited family and friends, and receive messages of support from loved ones – all from the palm of their hands.
Occupational Therapists help you resume activities of daily living (ADLs). We’ll help you return to life roles that have been interrupted by injury or disease. You’ll learn effective methods of approaching ADLs differently, including use of special equipment for lower body dressing, managing medication in the presence of declining memory or thought processes, and retraining to manage loss of hand or arm function due to stroke or other disabilities.
If you suffer from or have an increased risk of developing lymphedema, chronic swelling of the arms, legs, trunk, or head and neck, our Certified Lymphedema Therapist will help manage your condition through Complete Decongestive Therapy, which may include manual lymph drainage techniques, compression wrapping, skin care and exercise.
Our skilled Physical Therapists help rehabilitate and provide education to prevent disability following disease, injury, surgery, or loss of limb. We work hard to improve your strength and mobility by developing a treatment plan custom designed for you. We use therapeutic procedures to stretch and strengthen muscles and encourage return of motion. Our goal is to restore maximum movement and function to help you return to the lifestyle you desire

The goal of rehabilitation nursing is to assist individuals with disabilities and/or chronic illness to attain and maintain maximum function. Our rehabilitation nurses help patients and their families manage concerns like pain, skin care and bowel and bladder deficiencies during a stay on the rehab unit.
Rehab nurses teach and encourage patients to do as much as they can on their own with the goal for patients to do a little more each day.

Our certified and licensed speech-language pathologists are trained to evaluate and treat disorders that affect your speech, language, cognition and swallowing. Using personalized treatment plans we help you restore or improve your communication abilities and your cognitive function.
Our Speech Therapists are specialists in the evaluation and rehabilitation of swallowing disorders. If a patient’s condition requires it, the Speech-Language Pathologist or Physician may recommend a Modified Barium Swallow Study for diagnostic evaluation of swallow function.

As a current healthcare employee, Janelle was familiar around hospitals, but after an unexpected illness, she found herself in a new role: a patient.
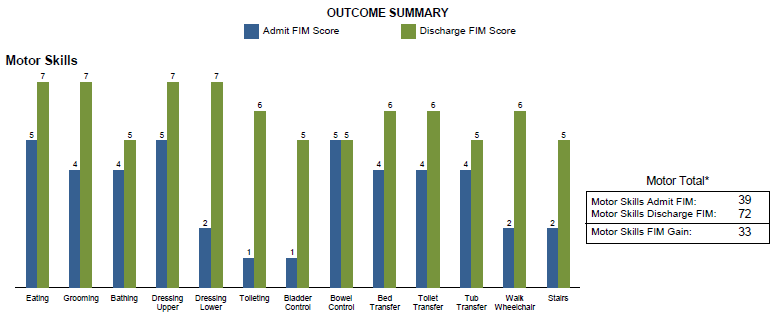
During her hospitalization, Janelle was diagnosed with respiratory failure requiring intubation and renal failure requiring dialysis. As a result of her long hospital stay Janelle was very weak and diagnosed with a critical illness myopathy, affecting her ability to function. Determined to be discharged to home, Janelle jumped at the opportunity to receive care on Hutchinson Regional’s Acute Rehab Unit.
At the beginning of rehab, Janelle faced many barriers, including dialysis and significant weakness affecting her ability to move. She focused on building her strength and regaining her independence.
After 16 days, Janelle went home using only a walker and no dialysis. “I credit Janelle’s progress to her hard work and motivation,” said Veronica Nail, PTA. “She had the heart and determination to go above and beyond to reach all of her goals. She was a joy to work with.”
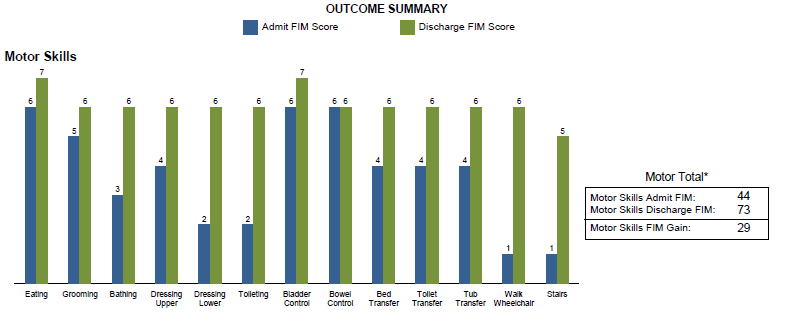
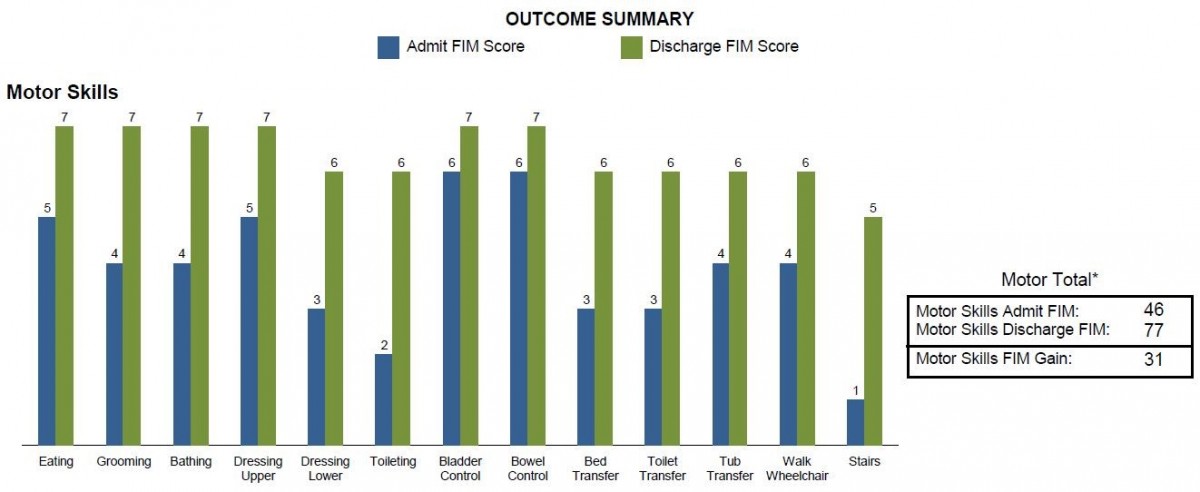
The Functional Independence Measure (FIM) instrument is a basic indicator of patient disability. FIM is used to track the changes in the functional ability of a patient during an episode of hospital rehabilitation care. A score of seven indicates that you are completely independent in that particular activity. A score of one means that you require total assistance for the activity.

When Frank was discharged from the hospital to a hospice facility, he really didn’t know what was going to happen. He was then transferred to inpatient rehab, and as the days passed, he began to get better and realized he still had a lot of fight left.
Frank began working with therapies and was able to regain enough strength to be able to be a patient at Hutchinson Regional’s Acute Rehab Unit. He wanted to get his life back.
At the beginning of rehab, Frank faced many barriers, including significant weakness and deconditioning affecting his ability to move. He focused on building his strength and tolerance to activity. As he continued to improve he not only met his goals, but surpassed them.
After 9 days Frank went home using only a walker and was walking further than he had in years. He credits his therapists and nurses with knowing how hard to push him. He said, “they made me work hard, but also knew when to let me rest.”

Susan has always been very active and a substitute teacher for 17 years. After a fall in her garden, she fractured her hip. After her surgery, Susan found herself in an unfamiliar situation. She was unable to care for herself safely and not able to return home.
During her hospitalization, Susan realized that she would be unable to return home due to the deficits from her fall and left hip fracture. Determined to be discharged to home, Susan jumped at the opportunity to receive care on Hutchinson Regional’s Acute Rehab Unit.
At the beginning of her rehab, Susan faced many barriers. The pain and weakness were affecting her ability to move. She remained focused on building her strength and regaining her independence.
After 7 days, Susan went home using only a walker. She really felt that going outside and simulating real life activites were very beneficial. It helped her feel prepared for a safe discharge. Regarding her stay Susan stated, “Rehab is the best place that a person can go after an injury.”
1701 E 23rd Ave
Hutchinson, KS 67502
620-665-2000
Visitation Hours:
M-F 6:00 am – 9:00 pm
Sat-Sun 7:00 am – 9:00 pm